Artlabeling Activity an Overview of Urine Formation the Nephron
The Urinary System
Physiology of Urine Formation
Learning Objectives
By the end of this section, you will be able to:
- Describe the hydrostatic and colloid osmotic forces that favor and oppose filtration
- Describe glomerular filtration rate (GFR), state the average value of GFR, and explain how clearance rate can be used to mensurate GFR
- Predict specific factors that will increase or decrease GFR
- State the pct of the filtrate that is ordinarily reabsorbed and explain why the procedure of reabsorption is so important
- Calculate daily urine product
- List common symptoms of kidney failure
Having reviewed the beefcake and microanatomy of the urinary organization, now is the time to focus on the physiology. You will discover that unlike parts of the nephron utilize specific processes to produce urine: filtration, reabsorption, and secretion. You lot will learn how each of these processes works and where they occur along the nephron and collecting ducts. The physiologic goal is to modify the composition of the plasma and, in doing and so, produce the waste material urine.
Failure of the renal anatomy and/or physiology tin can lead suddenly or gradually to renal failure. In this event, a number of symptoms, signs, or laboratory findings point to the diagnosis ((Effigy)).
| Symptoms of Kidney Failure |
|---|
| Weakness |
| Lethargy |
| Shortness of jiff |
| Widespread edema |
| Anemia |
| Metabolic acidosis |
| Metabolic alkalosis |
| Heart arrhythmias |
| Uremia (high urea level in the blood) |
| Loss of appetite |
| Fatigue |
| Excessive urination |
| Oliguria (too little urine output) |
Glomerular Filtration Charge per unit (GFR)
The volume of filtrate formed by both kidneys per minute is termed the glomerular filtration charge per unit (GFR). The middle pumps well-nigh five Fifty blood per min nether resting weather condition. Approximately 20 percent or one liter enters the kidneys to be filtered. On boilerplate, this liter results in the production of about 125 mL/min filtrate produced in men (range of 90 to 140 mL/min) and 105 mL/min filtrate produced in women (range of 80 to 125 mL/min). This amount equates to a book of most 180 L/twenty-four hour period in men and 150 L/day in women. Ninety-ix percent of this filtrate is returned to the circulation by reabsorption and so that only about i–2 liters of urine are produced per day ((Effigy)).
| Computing Urine Formation per Twenty-four hours | ||
|---|---|---|
| Flow per infinitesimal (mL) | Adding | |
| Renal blood flow | 1050 | Cardiac output is about 5000 mL/minute, of which 21 percent flows through the kidney. 5000*0.21 = 1050 mL claret/min |
| Renal plasma flow | 578 | Renal plasma flow equals the blood flow per minute times the hematocrit. If a person has a hematocrit of 45, and so the renal plasma flow is 55 pct. 1050*0.55 = 578 mL plasma/min |
| Glomerular filtration rate | 110 | The GFR is the amount of plasma entering Bowman's capsule per minute. It is the renal plasma menstruum times the fraction that enters the renal capsule (19 percent). 578*0.nineteen = 110 mL filtrate/min |
| Urine | 1296 ml/twenty-four hour period | The filtrate not recovered by the kidney is the urine that will be eliminated. It is the GFR times the fraction of the filtrate that is not reabsorbed (0.viii percentage). 110*.008 = 0.nine mL urine /min Multiply urine/min times 60 minutes times 24 hours to get daily urine production. 0.9*60*24 = 1296 mL/24-hour interval urine |
GFR is influenced by the hydrostatic force per unit area and colloid osmotic pressure on either side of the capillary membrane of the glomerulus. Recall that filtration occurs as pressure forces fluid and solutes through a semipermeable bulwark with the solute movement constrained past particle size. Hydrostatic pressure is the pressure produced by a fluid against a surface. If you have a fluid on both sides of a barrier, both fluids exert a pressure in opposing directions. Net fluid movement volition be in the direction of the lower pressure. Osmosis is the movement of solvent (water) across a membrane that is impermeable to a solute in the solution. This creates a pressure, osmotic pressure level, which will exist until the solute concentration is the same on both sides of a semipermeable membrane. As long equally the concentration differs, h2o will move. Glomerular filtration occurs when glomerular hydrostatic pressure exceeds the luminal hydrostatic pressure level of Bowman'south capsule. There is likewise an opposing forcefulness, the osmotic pressure, which is typically higher in the glomerular capillary.
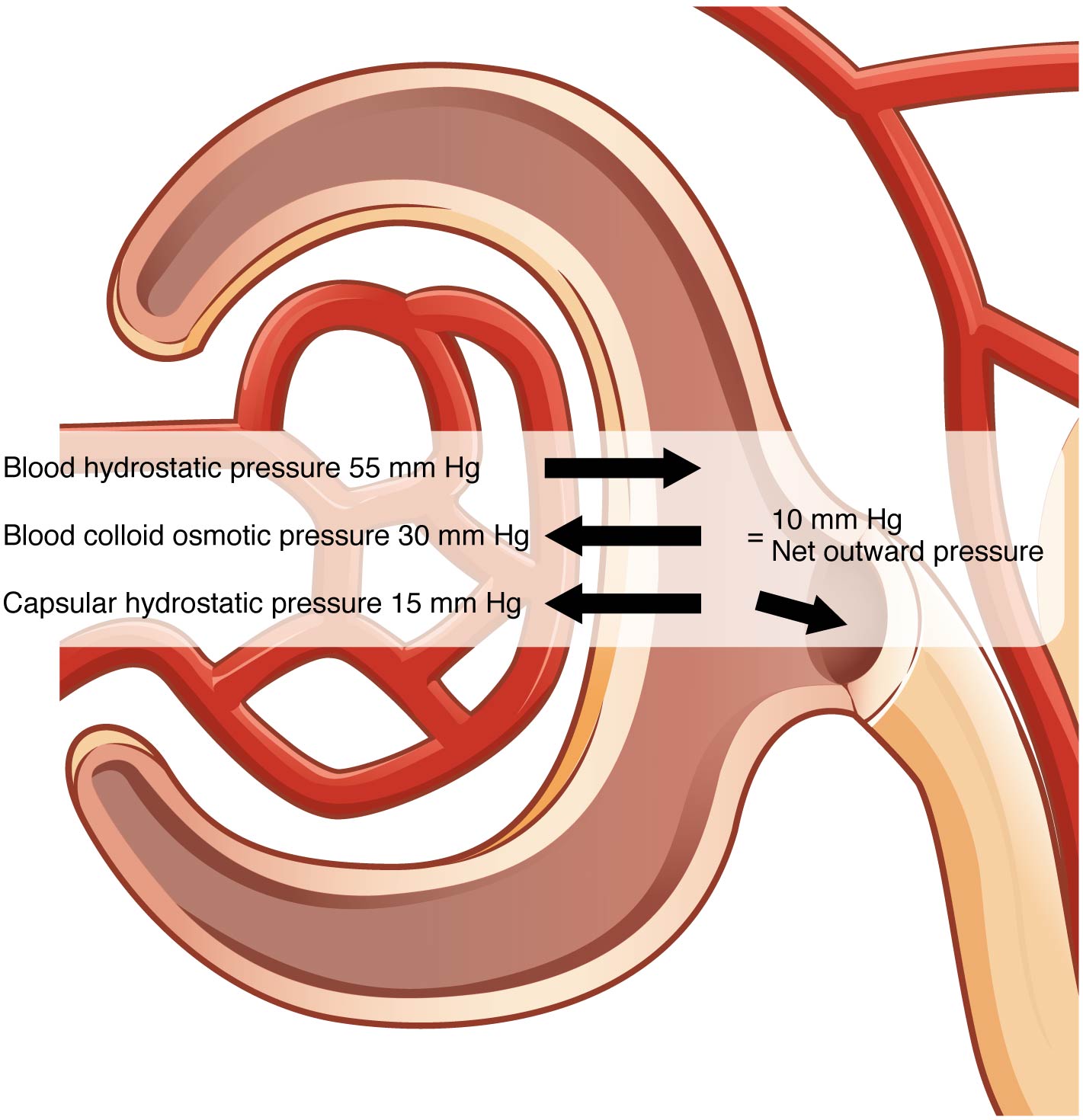
To understand why this is so, look more than closely at the microenvironment on either side of the filtration membrane. You will find osmotic pressure level exerted past the solutes inside the lumen of the capillary too as within of Bowman'due south sheathing. Since the filtration membrane limits the size of particles crossing the membrane, the osmotic pressure within the glomerular capillary is higher than the osmotic force per unit area in Bowman's capsule. Recall that cells and the medium-to-large proteins cannot pass betwixt the podocyte processes or through the fenestrations of the capillary endothelial cells. This means that red and white claret cells, platelets, albumins, and other proteins besides large to pass through the filter remain in the capillary, creating an average colloid osmotic force per unit area of thirty mm Hg within the capillary. The absenteeism of proteins in Bowman's infinite (the lumen inside Bowman's capsule) results in an osmotic pressure most nada. Thus, the only pressure moving fluid across the capillary wall into the lumen of Bowman's space is hydrostatic force per unit area. Hydrostatic (fluid) force per unit area is sufficient to button water through the membrane despite the osmotic force per unit area working confronting information technology. The sum of all of the influences, both osmotic and hydrostatic, results in a net filtration pressure (NFP) of most 10 mm Hg ((Figure)).
Net Filtration Pressure
The NFP is the sum of osmotic and hydrostatic pressures.
A proper concentration of solutes in the blood is of import in maintaining osmotic pressure level both in the glomerulus and systemically. There are disorders in which besides much protein passes through the filtration slits into the kidney filtrate. This excess protein in the filtrate leads to a deficiency of circulating plasma proteins. In turn, the presence of protein in the urine increases its osmolarity; this holds more h2o in the filtrate and results in an increase in urine volume. Because at that place is less circulating protein, principally albumin, the osmotic pressure of the claret falls. Less osmotic pressure pulling water into the capillaries tips the balance towards hydrostatic pressure level, which tends to push it out of the capillaries. The cyberspace effect is that water is lost from the apportionment to interstitial tissues and cells. This "plumps up" the tissues and cells, a condition termed systemic edema.
Cyberspace Filtration Pressure level (NFP)
NFP determines filtration rates through the kidney. It is determined equally follows:
NFP = Glomerular blood hydrostatic force per unit area (GBHP) – [capsular hydrostatic pressure (CHP) + blood colloid osmotic force per unit area (BCOP)] = 10 mm Hg
That is:
NFP = GBHP – [CHP + BCOP] = 10 mm Hg
Or:
NFP = 55 – [fifteen + 30] = 10 mm Hg
As y'all tin can meet, there is a low net pressure across the filtration membrane. Intuitively, you should realize that small changes in osmolarity of the blood or changes in capillary claret pressure result in major changes in the amount of filtrate formed at any given indicate in time. The kidney is able to cope with a wide range of blood pressures. In large part, this is due to the autoregulatory nature of shine muscle. When you stretch it, information technology contracts. Thus, when claret force per unit area goes up, smooth musculus in the afferent capillaries contracts to limit any increase in claret flow and filtration charge per unit. When blood force per unit area drops, the same capillaries relax to maintain claret flow and filtration charge per unit. The net consequence is a relatively steady flow of blood into the glomerulus and a relatively steady filtration charge per unit in spite of significant systemic blood pressure changes. Hateful arterial blood pressure is calculated by adding 1/3 of the departure between the systolic and diastolic pressures to the diastolic pressure level. Therefore, if the blood pressure is 110/80, the difference between systolic and diastolic pressure is 30. One tertiary of this is 10, and when you add this to the diastolic pressure of 80, you arrive at a calculated mean arterial pressure level of 90 mm Hg. Therefore, if y'all employ mean arterial pressure for the GBHP in the formula for calculating NFP, y'all tin can determine that as long every bit mean arterial force per unit area is above approximately 60 mm Hg, the pressure will exist adequate to maintain glomerular filtration. Blood pressures below this level volition impair renal function and cause systemic disorders that are severe enough to threaten survival. This status is called shock.
Determination of the GFR is one of the tools used to appraise the kidney'due south excretory function. This is more than just an academic exercise. Since many drugs are excreted in the urine, a decline in renal function can lead to toxic accumulations. Additionally, administration of appropriate drug dosages for those drugs primarily excreted by the kidney requires an accurate assessment of GFR. GFR tin can exist estimated closely by intravenous assistants of inulin. Inulin is a plant polysaccharide that is neither reabsorbed nor secreted by the kidney. Its appearance in the urine is directly proportional to the rate at which it is filtered past the renal corpuscle. Yet, since measuring inulin clearance is cumbersome in the clinical setting, most often, the GFR is estimated by measuring naturally occurring creatinine, a protein-derived molecule produced by muscle metabolism that is not reabsorbed and only slightly secreted by the nephron.
Affiliate Review
The entire book of the blood is filtered through the kidneys about 300 times per day, and 99 percent of the water filtered is recovered. The GFR is influenced past hydrostatic pressure and colloid osmotic pressure. Under normal circumstances, hydrostatic pressure is significantly greater and filtration occurs. The hydrostatic pressure level of the glomerulus depends on systemic claret pressure, autoregulatory mechanisms, sympathetic nervous activeness, and paracrine hormones. The kidney can function commonly under a broad range of blood pressures due to the autoregulatory nature of shine musculus.
Review Questions
________ pressure must be greater on the capillary side of the filtration membrane to attain filtration.
- Osmotic
- Hydrostatic
Production of urine to alter plasma makeup is the upshot of ________.
- filtration
- absorption
- secretion
- filtration, absorption, and secretion
Systemic blood pressure level must stay above 60 and then that the proper amount of filtration occurs.
- true
- false
Critical Thinking Questions
Give the formula for net filtration pressure level.
Net filtration force per unit area (NFP) = glomerular blood hydrostatic pressure (GBHP) – [capsular hydrostatic pressure (CHP) + blood colloid osmotic pressure level (BCOP)]
Proper name at to the lowest degree five symptoms of kidney failure.
Symptoms of kidney failure are weakness, languor, shortness of jiff, widespread edema, anemia, metabolic acidosis or alkalosis, heart arrhythmias, uremia, loss of appetite, fatigue, excessive urination, and oliguria.
Glossary
- glomerular filtration rate (GFR)
- rate of renal filtration
- inulin
- plant polysaccharide injected to determine GFR; is neither secreted nor absorbed by the kidney, so its appearance in the urine is directly proportional to its filtration charge per unit
- net filtration pressure (NFP)
- force per unit area of fluid beyond the glomerulus; calculated by taking the hydrostatic pressure of the capillary and subtracting the colloid osmotic force per unit area of the claret and the hydrostatic force per unit area of Bowman's sheathing
- systemic edema
- increased fluid retention in the interstitial spaces and cells of the body; can be seen as swelling over big areas of the body, especially the lower extremities
Source: https://opentextbc.ca/anatomyandphysiologyopenstax/chapter/physiology-of-urine-formation/
0 Response to "Artlabeling Activity an Overview of Urine Formation the Nephron"
Post a Comment